Colorectal Cancer Misdiagnosis Attorneys in Pennsylvania
Contact Frischman & Rizza Today
Frischman & Rizza, P.C.
Quick Facts
Colorectal cancer is the second leading cause of cancer-related deaths for both men and women combined.
Over 50% of all new cases of colon cancer involve metastatic spread to other organs and parts of the body at the time of diagnosis.
Approximately 50,000 Americans will die from colon cancer this year.
If colon cancer is detected and treated early, the survival rate is high.
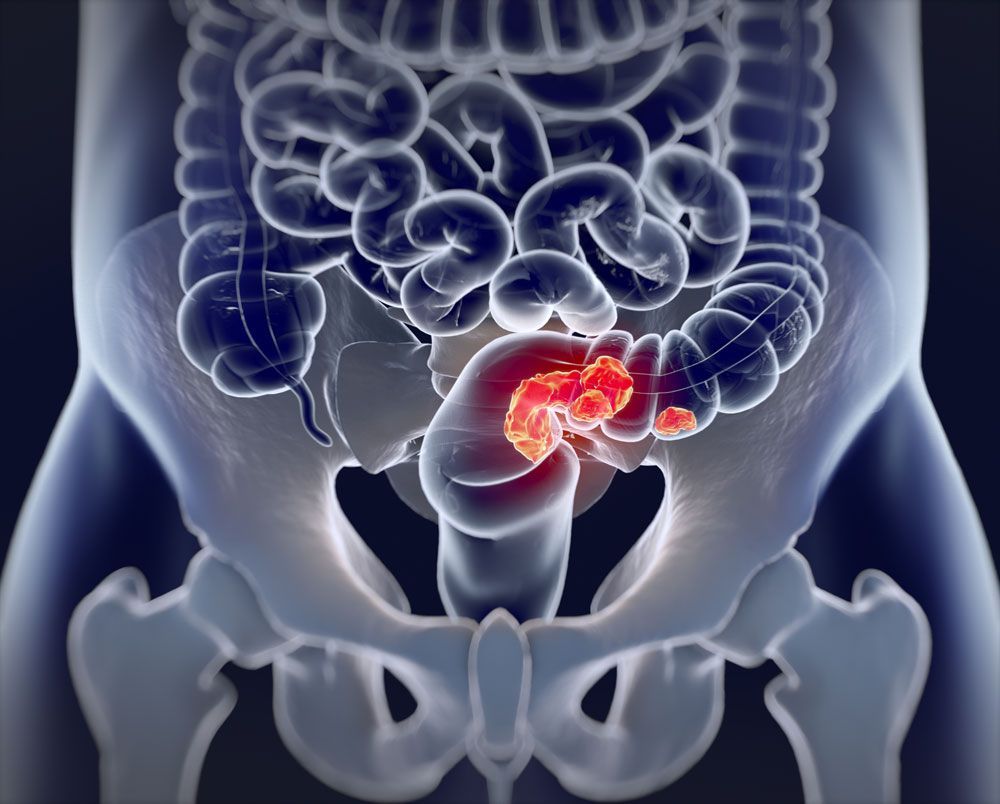
COLORECTAL CANCER MISDIAGNOSIS
Risk Factors
Risk factors of colon cancer include:
- Age 50 and older.
- Male 50 and older.
- Personal or family history of inflammatory condition in the intestines, such as Irritable Bowel Syndrome, Ulcerative Colitis or Chron’s Disease.
- A family history of colorectal cancer.
- Having a diet high in fat and low in fiber.
- Smoking tobacco.
Colorectal cancer is usually a slow-growing cancer that typically develops as pre-cancerous polyps in the lining of the colon. If the polyps are allowed to continue to grow and are not removed by either a colonoscopy or sigmoidoscopy some may become malignant (i.e., turn into colon cancer). Because colorectal cancer may become incurable once the disease has metastasized or spread outside the intestine, it is important for doctors to use early detection measures. Colorectal cancer misdiagnosis happens when there are clear signs that should have been detected by your medical professional, yet for some reason have gone unnoticed and untreated.
Common colorectal cancer symptoms include:
- Bloody stools.
- Change in bowel patterns.
- Narrow stool.
- Diarrhea or constipation.
- Gas pain.
However, colorectal cancer, especially in its early stages, often has no symptoms.
Cancer Misdiagnosis?
Contact our Colorectal Caner Misdiagnosis Attorneys at Frischman & Rizza for a free case evaluation.
Call Us On
Common Types of Colorectal Misdiagnosis & Malpractice
There are many reasons GI doctors and other health providers fail to properly diagnose colorectal cancer. These include:
- Cervical cancer
- Lung cancer
- Failing to recommend and/or order timely screening.
- Failing to respond to a patient’s complaints.
- Failing to detect cancer and remove polyps during the colonoscopy procedure.
- Failure of a family doctor to refer the patient to a GI doctor.
- Performing a colonoscopy on a patient who has not sufficiently cleaned his/her colon before the procedure.
Most cases of colon or rectal cancer are diagnosed in patients ages 55 to 84. Almost all colon cancers (95%) are adenocarcinomas. The balance of colon cancers include carcinoid tumors, lymphomas, melanomas, leiomyosarcomas or gastrointestinal stromal tumors.
American Cancer Society Updates Colorectal Cancer Screening Guidelines
The American Society (ACS) recently released an updated guideline for colorectal cancer screening (/cancer/colon-rectal-cancer/detection-diagnosis-staging/acs-recommendations.html). Among the major guideline changes, the new recommendations begin screening at age 45 (as opposed to age 50) for people at average risk for developing colorectal cancer.
For people of average risk, the ACS lowered the age to start screening after analyzing data from a major analysis led by ACS researchers (/latest-news/study-finds/sharp-rise-in-colon-cancer-and-rectal-cancer-rates-among-young-adults.html). This analysis revealed that new cases of colorectal cancer are occurring at an increasingly alarming rate among younger adults. After reviewing this data, experts on the ACS Guideline Development Committee concluded that a beginning screening age of 45 of adults of average risk for developing colorectal cancer will result in more lives saved.
New Screening Age Recommendations for Those at Average Risk
- People at average risk of colorectal cancer should start regular screening at age 45.
- People who are in good health and with a life expectancy of more than 10 years should continue regular colorectal cancer screening through the age of 75.
- Peoples ages 76 through 85 should make a decision with their medical provider about whether to be screened, based on their own personal preferences, life expectancy, overall health, and prior screening history.
- People over 85 should no longer get colorectal cancer screening.
Recommended Colorectal Cancer Screening Tests
Several test options are available for colorectal cancer screening:
- Stool-based tests:
- Highly sensitive fecal immunochemical test every year.
- Highly sensitive guaiac-based fecal occult blood test every year.
- Multi-targeted stool DNA test every 3 years.
- Visual exams:
- Colonoscopy every 10 years.
- CT colonography (virtual colonoscopy) every 5 years.
- Flexible sigmoidoscopy (FSIG) every 5 years.
The guidelines stress that these screening tests must be repeated at regular intervals to be effective. And, if you choose to be screened with a test other than colonoscopy, any abnormal test result must be followed up with a timely colonoscopy to complete the screening process.
- A strong family history of colorectal cancer or certain types of polyps (/cancer/colon-rectal-cancer/causes-risks-prevention/risk-factors.html)
- A personal history of colorectal cancer or certain types of polyps.
- A personal history of inflammatory bowel disease (ulcerative colitis or Crohn’s disease).
- A known family history of a hereditary colorectal cancer syndrome such as familial adenomatous polyposis (FAP).
- A personal history of radiation of the abdomen (belly) or pelvic area to treat prior cancer.
What about those at higher than average risk?
The guidelines also say that people at higher than average risk might need to start colorectal cancer screening before age 45, be screened more often, and/or get specific tests. People at higher or increased risk are those with:
- Strong family history: If you have a strong family history of colorectal cancer or certain types of polyps, your risk may be elevated. It's important to be aware of your family's medical history and discuss it with your healthcare provider.
- Personal history: If you have previously had colorectal cancer or certain types of polyps, your risk of developing the disease again is higher. Regular follow-up and monitoring are essential in these cases.
- Inflammatory bowel disease: Individuals with ulcerative colitis or Crohn's disease, which are types of inflammatory bowel disease, have an increased risk of colorectal cancer. Close monitoring and appropriate management are crucial in such situations.
- Hereditary colorectal cancer syndromes: A known family history of hereditary colorectal cancer syndromes, such as familial adenomatous polyposis (FAP), can significantly increase the risk of developing colorectal cancer. Genetic testing and counseling may be recommended in these cases.
- History of abdominal or pelvic radiation: If you have undergone radiation treatment in the abdomen or pelvic area for a previous cancer, it can increase the risk of developing colorectal cancer. Regular screenings and surveillance may be necessary for early detection.
If you believe you have undergone medical complications due to misdiagnosis, contact the attorneys at Frischman & Rizza today.


