National Practitioner Data Bank and Medical Malpractice Insights

Across the United States, a significant repository known as the National Practitioner Data Bank (NPDB) compiles information on civil lawsuits filed against doctors and other healthcare professionals for monetary damages. This database meticulously records instances where a healthcare provider has settled a medical malpractice lawsuit or faced disciplinary actions by state licensure bodies. While the NPDB holds potentially valuable information for patients researching their prospective doctors, access to this database is restricted to healthcare institutions for credentialing and licensure purposes, along with peer review organizations.
The Critical Nature of NPDB Claim Data
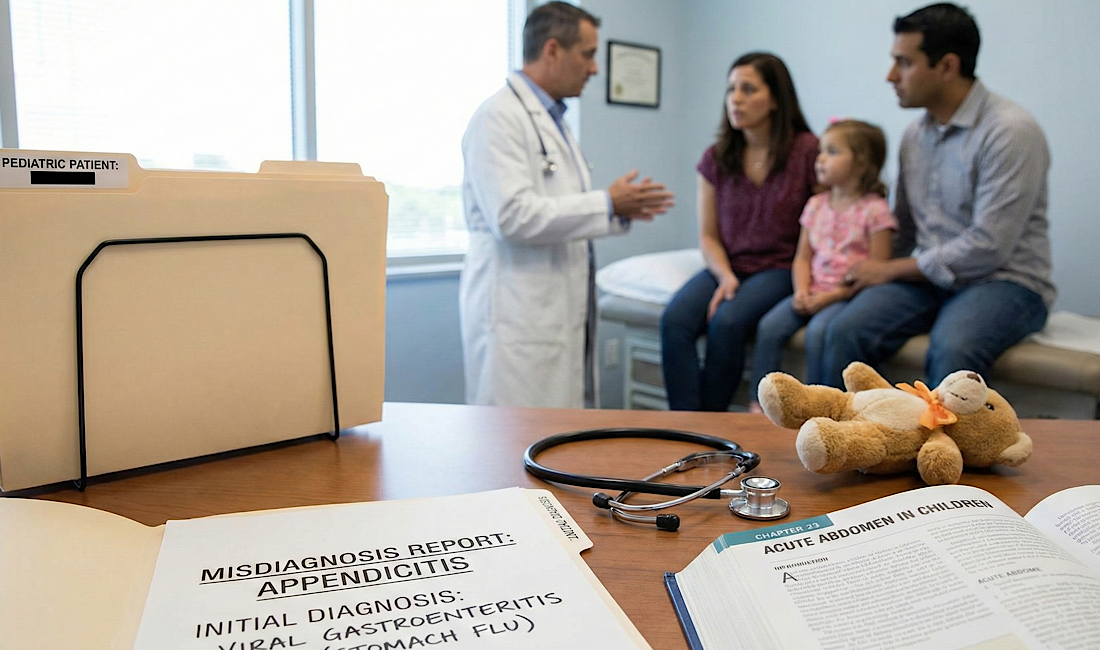
The inaccessibility of NPDB's claim data to the general public raises concerns, especially in light of studies indicating a correlation between doctors with previous
malpractice payouts and a higher likelihood of future claims. Such information could be crucial for patients when choosing a healthcare provider or considering surgery, suggesting a need for transparency in this area.
Debating the Privacy of NPDB Data
The debate around the NPDB's privacy hinges on the balance between professional confidentiality and the public's right to information. While medical organizations argue that public access could confuse patients and potentially increase insurance premiums, advocates for transparency believe it would enhance accountability within the medical profession and empower patients in their healthcare decisions.
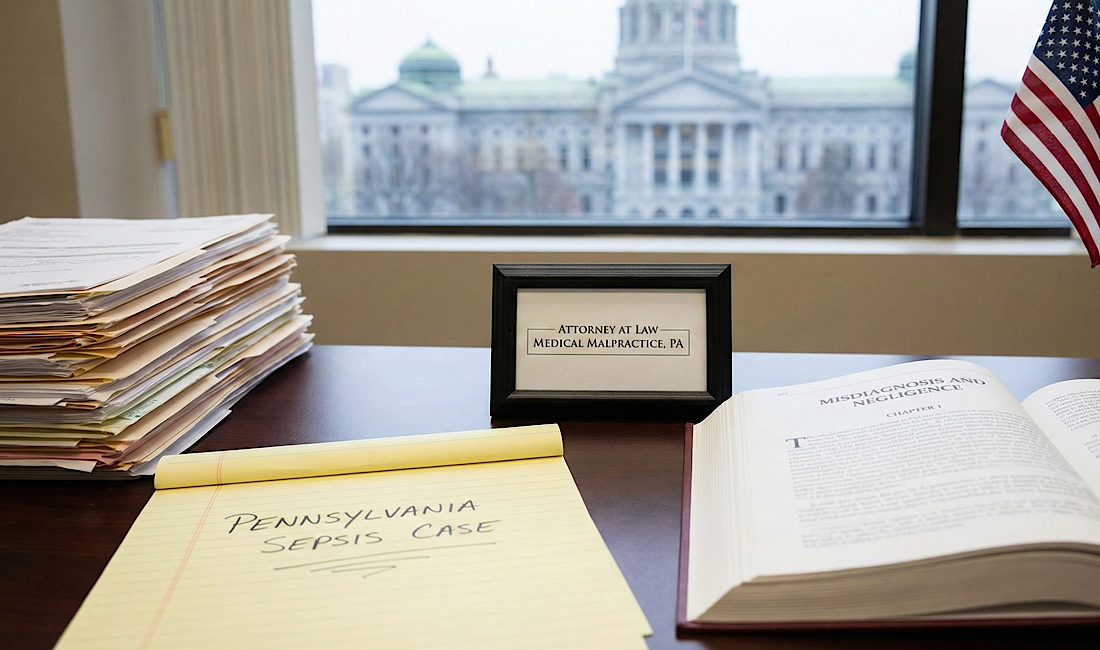
Seeking Legal Assistance for Medical Malpractice in Pennsylvania
Frischman & Rizza, P.C., stands out as a premier legal firm specializing in medical malpractice cases throughout Pennsylvania. Operating on a contingency basis, the firm assures clients that legal fees are only applicable upon securing a favorable verdict or settlement. The experienced legal team at Frischman & Rizza is dedicated to advocating for the rights of individuals affected by medical negligence, aiming to achieve justice and appropriate compensation for their clients.
If you've encountered medical malpractice in Pittsburgh or elsewhere in Pennsylvania, Frischman & Rizza offers a no-cost consultation to discuss your case, providing expert legal guidance to help you navigate your options.
For more information or to schedule a consultation, consider reaching out to
Frischman & Rizza, where the commitment to justice and client satisfaction is paramount.